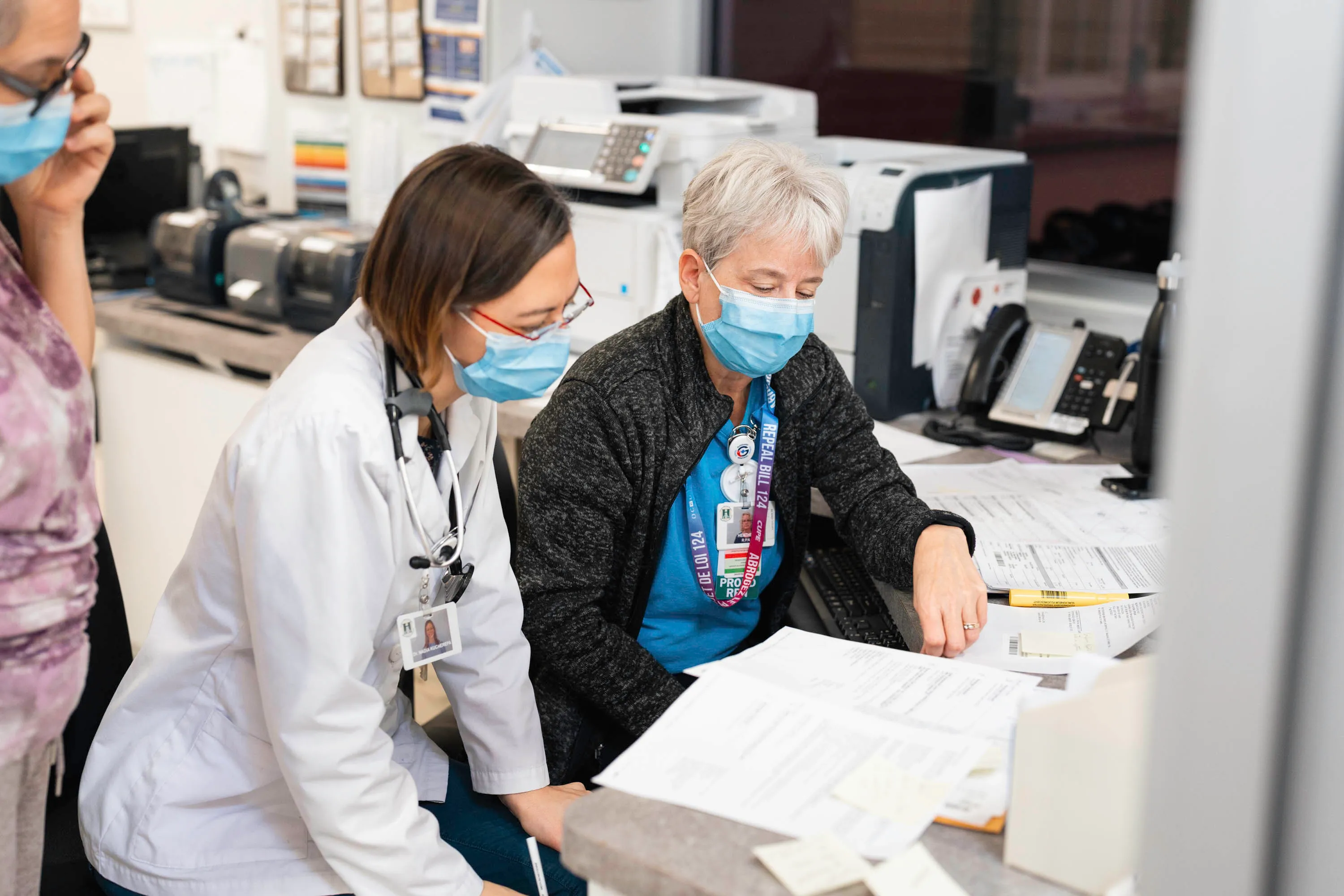
Essential Care Partner (ECP)

At HGMH, we understand that having a loved one around for our patients can be an essential part of healing. As such, we have introduced the Essential Care Partner (ECP) program. This page contains general information about the ECP Program at HGMH.
What is an Essential Care Partner (ECP)?
An Essential Care Partner (ECP) is a support person whose presence is considered essential to the safety and well-being of a patient while they are in the hospital. Most often, they are family or close friends of the patient who typically know the patient's health history, lifestyle, and personal values.
What is the difference between an Essential Care Partner and a Visitor?
Unlike a visitor, who plays a social role for the patient, ECPs provide a patient with essential support and function as a valued member of the care team.
How can an ECP support their loved ones?
There are many ways an ECP could offer support to their loved one. Some examples could include:
- advocating for them
- supporting their decision making
- providing emotional and cognitive support
- being a part of planning their care while in the hospital and once they are discharged
- helping them use technology to connect with friends of loved ones
- helping them eat, move around, bathe, communicate
- participating in patient and family education
- letting the care team know when they see a change in the patient
Who can choose an ECP?
All patients at HGMH (or their Substitute Decision Makers (SDM) can choose one ECP. However, not every patient will want or need an ECP. Ultimately, it is each patient's decision to make.
What are the expectations of an ECP?
ECPs will:
- always wear the ECP badge provided by the hospital for proper identification
- always follow hospital policies and infection prevention and control (IPAC) requirements.
- act as a partner with the care team
- provide updated information about the patient to the care team, especially any changes observed
- advise the unit if feeling unwell
ECPs will not:
- eat or drink in patient rooms
- use patient washrooms, public washrooms are available for use by the Main Entrance
- lift or transfer patients independently (without personalized training)
- administer medications (under any circumstances)
- enter the room of another patient
- provide care to another person
Your ECP Checklist
- Talk about your role with your loved one. Introduce yourself to staff. Describe your relationship to the patient and how you’d like to participate in care
- Observe changes (physical, behavioral, emotional) in the patient and report them to your loved one’s nurse. Ask staff what observations they would like you to routinely share
- Ensure that you’re present, if possible, at times when information will be shared, and decisions need to be made. Keep your schedule for coming to the hospital manageable. Let staff members know how to reach you and be sure you know whom to contact for information when you’re away from the bedside
- Help with decision-making about care and treatment. Be a second set of eyes and ears for the patient. Ask questions and take notes. Encourage your loved one to participate in decision-making to the extent they choose
- Ready yourself for the transition to home, Long Term, or Community Care. Before you leave the hospital, make sure your questions and those of the patient have been answered. Know what will be needed afterwards (medications, treatment, equipment, follow-up appointments) and what changes in the patient’s condition should be reported to health care providers
What are the steps to becoming an Essential Care Partner at HGMH?
- The patient or Substitute Decision Maker (SDM) chooses one person as their ECP
- The health-care team/clerk enters in the patient electronic medical record the name and contact information of the ECP
- The ECP must complete the following training on infection prevention and control (IPAC) practices.
i) Hand Hygiene
ii) Putting on Full PPE
iii) Taking off Full PPE
(If there are barriers to completing the online training, ECPs can access printed material or receive direct teaching from IPAC staff.) - The ECP agrees to follow IPAC practices and unit-specific policies. These can include physical distancing, hand washing, and wearing masks. Health-care staff must observe the ECP to ensure they are using personal protective equipment effectively.
For questions about Essential Care Partners, please talk to a member of the health care team.
Resource:
The Ontario Caregiver Organization